路 哥 Master
用 足 够 的 思 考 认 知 世 界

《柳叶刀》(The Lancet)创刊于1823年,由托马斯·威克利(Thomas Wakley)创刊的英国医学杂志。由爱思唯尔(Elsevier)出版公司主办,《柳叶刀》编辑部编辑出版的医学学术刊物 。是国际上公认的综合性医学四大期刊之一。
据2020年7月7日ScienceDirect显示,《柳叶刀》影响因子为59.102。据2020年7月7日《柳叶刀》杂志官网显示:《柳叶刀》根据2019年期刊引文报告与Clarivate Analytics 2020分析,影响因子为60.392。
作为国际最著名的期刊之一,其发布的信息和文章具有很强的权威性。本文转载和翻译近期由《柳叶刀》发布的一篇介绍Omicron的文章。可以看出,《柳叶刀》已经表达出了对新变种的担忧,但处于科学的态度和目前数据的不足,仍无法给出非常确定的结论。
(注意:标题用了“新篇章”这个词)
On Nov 25, 2021, about 23 months since the first reported case of COVID-19 and after a global estimated 260 million cases and 5.2 million deaths, a new SARS-CoV-2 variant of concern (VoC), omicron, was reported. Omicron emerged in a COVID-19-weary world in which anger and frustration with the pandemic are rife amid widespread negative impacts on social, mental, and economic wellbeing. Although previous VoCs emerged in a world in which natural immunity from COVID-19 infections was common, this fifth VoC has emerged at a time when vaccine immunity is increasing in the world.
2021年11月25日,自第一例新冠(COVID-19)报告以来约23个月,在全球估计2.6亿个病例和520万人死亡之后,报告了一个新的SARS-CoV-2变体(VoC),Omicron。Omicron出现在一个对新冠感到厌倦的世界中,在对社会、精神和经济福祉产生广泛负面影响的情况下,人们对这一流行病充满了愤怒和沮丧。虽然以前的变种出现在一个对新冠感染的自然免疫力很普遍的世界,但这第五个变种出现在世界疫苗免疫力正在增加的时候。
The emergence of the alpha, beta, and delta SARS-CoV-2 VoCs were associated with new waves of infections, sometimes across the entire world. For example, the increased transmissibility of the delta VoC was associated with, among others, a higher viral load, longer duration of infectiousness, and high rates of reinfection, because of its ability to escape from natural immunity, which resulted in the delta VoC rapidly becoming the globally dominant variant. The delta VoC continues to drive new waves of infection and remains the dominant VoC during the fourth wave in many countries. Concerns about lower vaccine efficacy because of new variants have changed our understanding of the COVID-19 endgame, disabusing the world of the notion that global vaccination is by itself adequate for controlling SARS-CoV-2 infection. Indeed, VoCs have highlighted the importance of vaccination in combination with existing public health prevention measures, such as masks, as a pathway to viral endemicity.
Alpha、Beta和Delta SARS-CoV-2 变种的出现与新的感染浪潮有关,有时甚至跨越整个世界。例如,Delta变种的传播性增加,与更高的病毒量、更长的传染性和高再感染率有关,因为它有能力逃避自然免疫,这导致delta变种迅速成为全球的主导变体。德尔塔型病毒感染者继续推动新的感染浪潮,在许多国家的第四浪潮中仍然是主要的病毒感染者。对新变异体导致疫苗效力降低的担忧改变了我们对新冠终局的理解,使世界不再认为全球疫苗接种本身就足以控制新冠变种感染。事实上,多个变种已经强调了疫苗接种与现有公共卫生预防措施(如口罩)相结合的重要性,这是一条通往病毒流行的途径。
The first sequenced omicron case was reported from Botswana on Nov 11, 2021, and a few days later another sequenced case was reported from Hong Kong in a traveller from South Africa. Several sequences from South Africa followed, after initial identification that the new variant was associated with an S-gene target failure on a specific PCR assay because of a 69–70del deletion, similar to that observed with the alpha variant. The earliest known case of omicron in South Africa was a patient diagnosed with COVID-19 on Nov 9, 2021, although it is probable that there were unidentified cases in several countries across the world before then. In South Africa, the mean number of 280 COVID-19 cases per day in the week before the detection of omicron increased to 800 cases per day in the following week, partly attributed to increased surveillance. COVID-19 cases are increasing rapidly in the Gauteng province of South Africa; the early doubling time in the fourth wave is higher than that of the previous three waves (figure).
2021年11月11日,博茨瓦纳报告了第一个测序的Omicron病例,几天后,香港报告了另一个测序的病例,是一个来自南非的旅行者。随后,来自南非的几个序列,经过初步鉴定,新的变体与特定PCR检测中的S基因靶点失败有关,因为有一个69-70del的缺失,与观察到的α变体相似。在南非已知的最早的Omicron病例是2021年11月9日被诊断为新冠的患者,尽管在此之前可能在全球多个国家有未被识别的病例。在南非,在检测到奥米隆之前的一周,平均每天有280例COVID-19病例,在接下来的一周增加到每天800例,部分原因是加强了监测。新冠病例在南非的豪登省迅速增加;第四波的早期翻倍时间高于前三波(下图)。
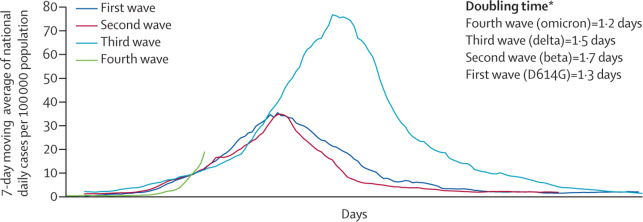
FigureSARS-CoV-2 cases in first, second, third, and fourth waves, Gauteng Province of South Africa
The principal concerns about omicron include whether it is more infectious or severe than other VoCs and whether it can circumvent vaccine protection. Although immunological and clinical data are not yet available to provide definitive evidence, we can extrapolate from what is known about the mutations of omicron to provide preliminary indications on transmissibility, severity, and immune escape. Omicron has some deletions and more than 30 mutations, several of which (eg, 69–70del, T95I, G142D/143–145del, K417N, T478K, N501Y, N655Y, N679K, and P681H) overlap with those in the alpha, beta, gamma, or delta VoCs. These deletions and mutations are known to lead to increased transmissibility, higher viral binding affinity, and higher antibody escape. Some of the other omicron mutations with known effects confer increased transmissibility and affect binding affinity. Importantly, the effects of most of the remaining omicron mutations are not known, resulting in a high level of uncertainty about how the full combination of deletions and mutations will affect viral behaviour and susceptibility to natural and vaccine-mediated immunity.
对Omicron的主要关注包括它是否比其他变种更具传染性或更严重,以及它是否能规避疫苗保护。尽管目前还没有免疫学和临床数据来提供确切的证据,但我们可以从已知的omicron的突变中推断出关于传播性、严重性和免疫逃避的初步迹象。Omicron有一些缺失和30多个突变,其中有几个(如69-70del、T95I、G142D/143-145del、K417N、T478K、N501Y、N655Y、N679K和P681H)与α、β、γ或δVoCs中的突变重叠。这些缺失和突变已知会导致传播性增加,病毒结合亲和力提高,抗体逃逸率提高。其他一些具有已知影响的微米级突变会增加传播性并影响结合亲和力。重要的是,剩下的大多数微观突变的影响尚不清楚,这导致了高度的不确定性,即删除和突变的全部组合将如何影响病毒行为和对自然和疫苗介导的免疫的敏感性。
The impact of omicron on transmissibility is a concern. If the overlapping omicron mutations maintain their known effects, then higher transmissibility is expected, particularly because of the mutations near the furin cleavage site. Early epidemiological evidence suggests that cases are rising in South Africa and that PCR tests with S-gene target failure are also rising. Although omicron is likely to be highly transmissible, it is not yet clear whether it has greater transmissibility than delta, although preliminary indications suggest that it is spreading rapidly against a backdrop of ongoing delta-variant transmission and high levels of natural immunity to the delta variant. If this trend continues, omicron is anticipated to displace delta as the dominant variant in South Africa.
Omicron对传播性的影响是一个值得关注的问题。如果重叠的Omicron突变保持其已知的影响,那么预计会有更高的传播性,特别是由于靠近furin裂解位点的突变。早期的流行病学证据表明,南非的病例正在上升,S基因目标失败的PCR检测也在上升。尽管Omicron可能具有高度的传播性,但尚不清楚它是否比delta具有更大的传播性,尽管初步迹象表明,在Delta变异体持续传播和Delta变异体具有高度自然免疫力的背景下,它正在迅速蔓延。如果这种趋势继续下去,预计Omicron将取代Delta成为南非的主要变体。
We await knowledge of how this new VoC will impact clinical presentation. At this stage, the available anecdotal data from clinicians at the front lines in South Africa suggest that patients with omicron are younger people with a clinical presentation similar to that of past variants. Although no alarming clinical concerns have been raised thus far, this anecdotal information should be treated with caution given that severe COVID-19 cases typically present several weeks after the initial symptoms associated with mild disease.
我们正在等待关于这种新的变种将如何影响临床表现的知识。在这个阶段,来自南非前线临床医生的现有传闻数据表明,Omicron患者是年轻人,其临床表现与过去的变体相似。尽管到目前为止还没有提出令人震惊的临床问题,但鉴于严重的新冠病例通常在与轻度疾病相关的初始症状出现后数周才出现,因此应谨慎对待这一传闻信息。
Immune escape is another concern. In the absence of data on observational vaccine effectiveness and antibody-neutralisation studies on vaccinee sera, preliminary data from the national PCR testing programme could provide some clues. Data on positive PCR tests in people with previous positive tests suggest an increase in cases of reinfection in South Africa. However, the increased use of rapid antigen tests and incomplete capturing of negative results have complicated the interpretation of test positivity rates, which have risen to about four times the previous rate in the past week. Notwithstanding this limitation, the increase in cases of reinfection is in keeping with the immune-escape mutations present in omicron.
免疫逃逸是另一个问题。由于缺乏关于疫苗有效性的观察数据和对被接种者血清的抗体中和研究,来自国家PCR检测计划的初步数据可以提供一些线索。之前PCR检测呈阳性的人的数据表明,南非的再感染病例在增加。然而,快速抗原检测的使用增加和对阴性结果的不完全捕捉使检测阳性率的解释变得复杂,在过去的一周里,阳性率已经上升到以前的四倍左右。尽管有这种局限性,但再感染病例的增加与欧米茄中存在的免疫逃逸突变是一致的。

Although there are conflicting reports on whether COVID-19 vaccines have consistently retained high efficacy for each of the four VoCs preceding omicron, clinical trials have reported lower efficacy for some vaccines in transmission settings in which the beta variant is dominant. Previous variants have lowered vaccine efficacy; for example, the ChAdOx1 vaccine was 70% effective in preventing clinical infections for the D614G variant in the UK, but this efficacy decreased to 10% for the beta variant in South Africa. However, the efficacy of the BNT162b2 vaccine in preventing clinical infections was retained across both the D614G and beta variants. Given that omicron has a larger number of mutations than previous VoCs, the potential impact of omicron on the clinical efficacy of COVID-19 vaccines for mild infections is not clear.
尽管关于新冠疫苗是否始终保持对Omicron之前的四种VoC的高效力的报告存在冲突,但临床试验报告显示,在β变体占主导地位的传播环境中,一些疫苗的效力较低。以前的变体降低了疫苗效力;例如,在英国,ChAdOx1疫苗对D614G变体的临床感染有70%的预防效果,但在南非,这一效力对β变体下降到10%。然而,BNT162b2疫苗在预防临床感染方面的功效在D614G和β变体中都得以保留。鉴于Omicron比以前的VoC有更多的突变,Omicron对新冠疫苗对轻度感染的临床疗效的潜在影响尚不清楚。
Thus far, most COVID-19 vaccines have remained effective in preventing severe COVID-19, hospitalisation, and death, for all previous variants, because this efficacy might be more dependent on T-cell immune responses than antibodies. Observational studies from Qatar (n=231 826) and Kaiser Permanente (n=3 436 957) reported vaccine efficacy of more than 90% in preventing hospital admissions during delta-variant transmission, even up to 6 months after vaccination. Observational data from the state of New York, USA (n=8 834 604) indicated high vaccine efficacy in preventing severe disease in people older than 65 years, with varying levels of protection conferred by different vaccines—95% for BNT162b2, 97% for mRNA-1273, and 86% for Ad26.COV2.S—with minimal declines in protection 6 months after vaccination.
到目前为止,大多数新冠疫苗在预防严重的新冠、住院治疗和死亡方面仍然有效,对于以前的所有变种,因为这种功效可能更依赖于T细胞免疫反应而不是抗体。来自卡塔尔(n=231 826)和Kaiser Permanente(n=3 436 957)的观察性研究报告称,在delta变异体传播期间,疫苗预防入院的功效超过90%,甚至在接种疫苗后6个月。来自美国纽约州的观察数据(n=8 834 604)表明,在预防65岁以上人群的严重疾病方面,疫苗的效力很高,不同疫苗的保护程度不同--BNT162b2为95%,mRNA-1273为97%,Ad26.COV2.S为86%--接种6个月后,保护程度下降很小。
In terms of diagnostics, the omicron variant is detectable on widely used PCR platforms in South Africa. There is no reason to believe that current COVID-19 treatment protocols and therapeutics would no longer be effective, with the possible exception of monoclonal antibodies, for which data on the omicron variant's susceptibility are not yet available. Importantly, existing public health prevention measures (mask wearing, physical distancing, avoidance of enclosed spaces, outdoor preference, and hand hygiene) that have remained effective against past variants should be just as effective against the omicron variant.
在诊断方面,在南非广泛使用的PCR平台上可以检测到Omicron变体。没有理由相信目前的新冠治疗方案和治疗方法会不再有效,但单克隆抗体可能是个例外,目前还没有关于Omicron变体敏感性的数据。重要的是,现有的公共卫生预防措施(戴口罩、保持身体距离、避免进入封闭空间、户外活动、手部卫生)对过去的变体仍然有效,应该对Omicron变体也同样有效。
Extrapolations based on known mutations and preliminary observations, which should be interpreted with caution, indicate that omicron might spread faster and might escape antibodies more readily than previous variants, thereby increasing cases of reinfection and cases of mild breakthrough infections in people who are vaccinated. On the basis of data from previous VoCs, people who are vaccinated are likely to have a much lower risk of severe disease from omicron infection. A combination prevention approach of vaccination and public health measures is expected to remain an effective strategy.
基于已知突变和初步观察的推断(应谨慎解释)表明,与以前的变体相比,Omicron可能传播得更快,而且可能更容易逃避抗体,从而增加再感染的病例和接种疫苗者的轻度突破性感染病例。根据以前的变种数据,接种疫苗的人可能会大大降低Omicron感染的严重疾病风险。疫苗接种和公共卫生措施相结合的预防方法预计仍将是一项有效的战略。
( 结 束 )
发表评论